Scientists at the Luxembourg Institute of Health (LIH) have discovered a previously unknown molecular mechanism that promotes activation of the human immune system, opening a door to new strategies for targeting cancer and autoimmune diseases.
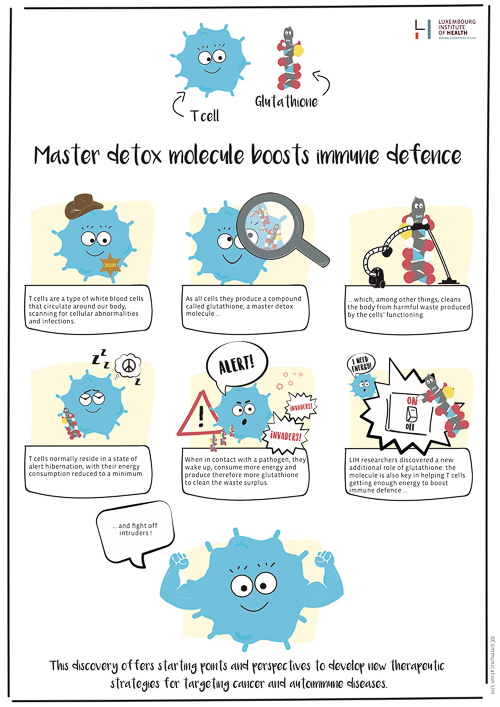
The team, led by Professor Dirk Brenner, fellow and head of the Experimental & Molecular Immunology research group, has been studying the glutathione molecule, produced among others by a particular type of white blood cells named T-cells and known for its role in cleaning the body from harmful metabolic wastes. Their research project revealed that glutathione also stimulates T-cells’ metabolic energy.
“Our body has to keep our immune system in a carefully balanced equilibrium,” said Professor Brenner. “If the body’s innate defences are overactive, then they turn against the body. This is what happens in autoimmune diseases like multiple sclerosis or arthritis, for example.
“However if the defences are too weak, then infections cannot be handled or body cells can proliferate uncontrolled and grow to form tumours, which can become life threatening.”
Immune cells such as T-cells therefore normally reside in a state of alert hibernation, with their energy consumption reduced to a minimum. If pathogens come into contact with the T-cells, these wake up and boost their metabolism to produce more energy. This necessarily creates greater amounts of metabolic waste products such as reactive oxygen species (ROS) and free radicals, which can be toxic for the cells.
When the concentration of these oxidants increases, the T-cells have to produce more antioxidants so as not to be poisoned. No previous research group had studied the mechanism of action of antioxidants in T-cells to great detail before. In exploring this phenomenon, Professor Brenner’s team discovered that the antioxidant glutathione produced by T-cells serves not only as a garbage collector to dispose of metabolic waste products, it is also a key switch for energy metabolism that controls the immune response, and is thus of high relevance to various diseases.
“These fascinating results form a basis for a targeted intervening in the metabolism of immune cells and for developing a new generation of immuno-therapies,” said Professor Markus Ollert, Director of LIH’s Department of Infection and Immunity.
For their investigations, the scientists employed animal models having T-cells unable to produce glutathione. “In these mice, we discovered that the control of viruses is impaired – these mice have an immunodeficiency. But by the same token, this also meant the mice could not develop any autoimmune disease such as multiple sclerosis.” Further tests performed by Professor Brenner’s team demonstrated the reason for this.
“The mice cannot produce any glutathione in their T-cells,” said Professor Brennor. “As a result, without glutathione, T-cells do not become fully functional; they remain in their state of hibernation and no self-destructive autoimmune response occurs.”
Professor Karsten Hiller from the Braunschweig University of Technology, who collaborated with the Luxembourgish scientists added, “It is intriguing to see that cellular metabolism and immune activation are so tightly entangled and that a fine-grained interplay is essential to achieve a correct function."
Professor Brenner sees his T-cell experiments as a prelude to more in-depth investigation of the energy balance of immune cells in general. A number of different autoimmune diseases, for example, are related to malfunctions in various subgroups of T-cells.
“If we understand the differences in the molecular mechanisms by which they stimulate their metabolism to get energy during defensive or autoimmune responses, then we can discover clues as to possible attack points for therapeutic agents regulating the immune response.”
The researcher sees a similar situation in cancer. “In this context too, it is important to know why the immune cells that are actually supposed to fight cancer cells drop to a low metabolic state and in some cases even actively suppress an immune response against the tumour. Counteractive metabolism-stimulating measures could make the immune cells work more efficiently and fight off cancer more effectively,” he said.
In follow-up projects, the researchers are planning to gain new indications for potential sites of therapeutic interventions. The groups from Luxembourg and Braunschweig are currently applying for new research funding for a joint project supported by the German Research Foundation (DFG) and the Luxembourg National Research Fund (FNR).
The scientists publish their findings today in the world’s most prestigious immunology journal, “Immunity” (DOI: 10.1016/j.immuni.2017.03.019.).
Image: © Communication LIH








